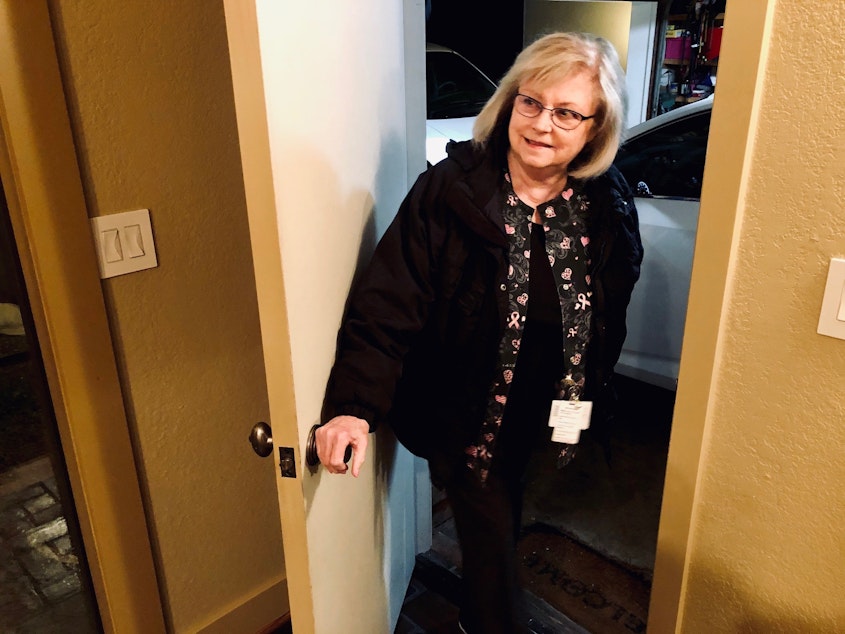
My 71-year-old mom is a nurse on the front lines of COVID-19. I’m worried. She’s not.

I asked her if she feels scared going to work since the coronavirus outbreak. She said if nurses are afraid, they won't be able to do their jobs.
My mom has been a hospital nurse for 49 years. Her name is Kathy Leong. She’s a full-time medical-surgical nurse at a hospital in Bellevue, just east of Seattle. She’s only a few miles from the Kirkland nursing home that has been the epicenter of the COVID-19 initial outbreak in the United States.
Because of my mom’s age, her manager has exempted her (as well as immunocompromised and pregnant nurses on their unit) from caring for COVID-19-positive patients directly. But those patients are on my mom’s unit. And even if she’s not directly in contact with infected patients, she and the other exempt nurses are working closely with the nurses who are treating them, being even more attentive than usual as they support their overworked colleagues.
Overloaded nurses and changing rules leads to tension
For the nurses who are caring for patients with coronavirus, their workloads and risks have significantly increased. There’s tension on the unit between the nurses that wasn’t there before. The stress is palpable.
Almost every day the nurses on my mom’s unit report to work, the expectations have changed. New protective protocols are added or removed. Guidelines are shifted as the hospital learns more about this virus, or because of a recommendation or order from the governor or CDC. Patients are admitted in waves, their conditions and needs varying widely.
Sponsored
Just the other day, nurses on my mom’s unit were covered from head to shoulders with a yellow tent-like contraption. Scents were blown into the tents while the nurses donned N95 face masks. The hospital was fitting the nurses to the new masks, making sure they couldn't smell or taste the scents blown into the tents. Life is not business as usual for nurses during this pandemic.
For my mom though, she says this is all just part of the job. When I asked her if she’s felt any regret about becoming a nurse since the coronavirus has broken out, she said no. Actually, she said, “Oh heavens, no. No no no no no no no.”
Nursing has changed a lot over the last 50 years
My mom has wanted to be a nurse since she was five-years-old. Although nursing has changed a lot over the past five decades, she still loves it.
As a new nurse in the 1970’s, she said some patients would come in for a few weeks because their doctors had told them “they just needed a rest.” They’d bring books and flowers and settle in for a rejuvenating break. Were those patients annoying? Absolutely. But they weren’t uncommon.
Sponsored
These days, patients in hospitals are in serious condition. Fearful of spreading the virus and facing inadequate numbers of healthcare providers to treat the exponentially growing number of coronavirus patients, hospitals across the country are delaying elective surgeries and urging people to stay away except for emergencies. Masks and beds are in short supply. At my mom’s hospital, they’ve begun talking about reinforcing cloth masks with surgical drape sheets.
Patients and human connections lost in this pandemic
Even though space is scarce, my mom says some nursing homes won’t allow their residents to return even after they’ve recovered from COVID-19. The last she heard, those patients are required to test negative for the virus twice before being able to return home. That takes extra time, money, and more tests, which are also in short supply in Washington state, where coronavirus has been confirmed to have infected 2,221 people and killed 110 as of the writing of this story.
Meanwhile, others who are ill but not infected with coronavirus, are being seemingly sidelined in the chaos of this pandemic. Last week, one of my mom’s patients lost his battle with cancer. My mom’s a tough lady. When she talks about her work, she’s matter-of-fact, all business. But as she told me about this patient, she became uncharacteristically wistful. Quietly, she said his death seemed secondary.
Sponsored
“You can’t go up and hug a patient or hug a family if they’re grieving,” she told me sadly, referencing the hospital’s effort to enact the six feet social distancing recommendation.
“I don’t like it,” she concluded. “But we do it. We do what we have to do.”
To listen to my 3.5 minute story featuring my mom reflecting on 49 years of nursing and what it’s like to be a caregiver who can’t give hugs during this pandemic, click the play arrow in the upper right corner.
If you believe you have been exposed to COVID-19, or are a healthcare provider with questions about COVID-19, contact King County's novel coronavirus call center at 206-477-3977 between 8 a.m. and 7 p.m. People can also call the Washington State Novel Coronavirus Call Center at 800-525-0127.




