Syphilis infections on the rise in Seattle area
Syphilis infections are rising quickly in the Puget Sound region, and nationwide, spread through sex, often asymptomatically.
But in a strange twist, increasing syphilis rates are also an indication of success against a different problem – HIV.
Talking about sex can be pretty awkward, especially when it relates to sexually transmitted infections. So I decided to stand outside bars on a Friday night wearing a giant sign that said, “Let’s talk about queer sex for the radio.”
“I love queer sex!” one passerby shouts, ensconced in their entourage.
On assignment with me is Chris Porter, a nurse and health messaging coordinator with POCAAN, or People of Color Against AIDS Network. He came along to answer questions and provide medical facts (and free condoms).
We approach partiers, explain the story, and hand people graphs with data on syphilis trends.
What, that’s not how you bar hop?
Sponsored
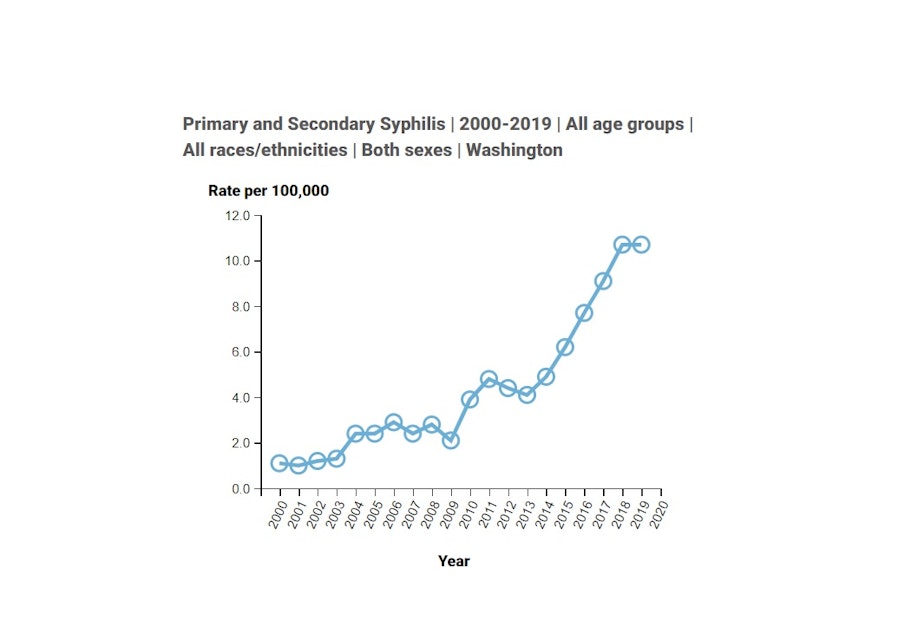
Treponema pallidum, which causes syphilis, has grown to be about 10 times more common in Washington state today compared to 20 years ago, with close to a thousand cases found each year.
“Holy moly!” Robert Steinfelder said.
He and Gabriel Mora were out for the evening in Seattle’s Capitol Hill when we engaged them in conversation, and they want to understand why.
Porter explains that one of the reasons syphilis has gone up is because another sexually transmitted infection, HIV, has gone down. Nowadays, medicines exist to prevent and suppress HIV and keep it from spreading, so some people have more sex without condoms.
“It's easy for many to forget that while they're taking this very potent medication to prevent HIV, not using a condom still does not protect you against chlamydia, gonorrhea, and syphilis,” Porter says.
Sponsored
Since 2000, chlamydia rates have increased 85% to more than 31,000 cases in 2020 in Washington. Gonorrhea rates have almost quadrupled to more than 11,000 cases, according to data from the Centers for Disease Control and Prevention and the Washington State Department of Health.
In front of a different bar, we talk with Tyler Wong, a gay man in his late 20s who is on PrEP, or pre-exposure prophylaxis, the medication that prevents HIV infection.
“With the gay community and PrEP now, I feel like there's a lot less fear,” he said. “So there's a lot more openness to adventure and try stuff out.”
That sexual freedom feels good.
“I feel like sex shouldn’t have to be a scary thing, so it’s nice that you can have sex without as much consequence,” he said, and adds that the risk of STIs makes it especially important to get checked regularly.
Sponsored
(For a list of testing providers in King County visit here.)
Wong gets tested every three months by routine.
“Sometimes it's like going to the dentist. I'm like, ‘Oh, am I gonna have a cavity?’ Going to the doctor it’s like, ‘Am I gonna have an STI?’" Wong said.
“It's not the end of the world” if the test shows something, he said.
Indeed, one shot of penicillin can treat syphilis if you find it early. But as time goes on you need more treatment, you can spread it to others, and the disease can progress in dangerous and devastating ways.
Sponsored
Unannounced syphilis
Untreated, syphilis can royally screw up your body, from hair loss and blindness to stroke or psychosis.
That’s what Chris, the nurse, tells another young man we met, who doesn’t give his name. The guy says he “doesn’t really” use condoms and gets tested once a year.
“If you are regularly sexually active, once a year testing puts you waaaayyy behind,” Chris says.
“In that case, I’m not regularly active. Once every two months!” the man says, giggling nervously.
Sponsored
“If I may…” Chris begins. “If you only test once a year and you became infected with syphilis, in that year, it has an opportunity to get into your nervous system.”
“Ah, that’s fucked up,” the man says.
“Yeah,” Chris says. “That's called neurosyphilis. Which you don't want to get.”
Chris warns the folks we meet about syphilis’ potential to spread asymptomatically. Sometimes you might see a sore where the bacteria entered your body – for example, your mouth, genitals or rectum – or you may have a rash on parts of your body, such as your palms or soles of your feet.
The CDC has a whole online database of many NSFW examples of what that looks like.

But often, a visit from syphilis goes unannounced.
“Many times there are few or no symptoms, and the symptoms appear and then go away whether you get treated or not,” Chris says.
The rates tend to be highest among Black, Indigenous and people of color and men who have sex with men. That’s why I used the phrase “queer sex” on my sign to try to find people who might have direct experience with the issues in this story.
Rising syphilis in King County
However, now more men and women having sex together are starting to get infected too. That makes public health officials especially concerned because pregnant people can pass syphilis on to their babies.
Cases of congenital syphilis, as it’s called, have risen dramatically in King County. For many years there were none, but last year there were at least 10, according to Public Health – Seattle and King County.
“It’s a big deal,” said Matthew Golden, who directs the HIV and STD program at Public Health – Seattle & King County. Syphilis in babies can be devastating.
“That can lead to death of the baby, it can lead to neurological complications in the baby,” he said. “This is what we want to avert, I would say more than anything.”
Many of the mothers in recent cases were homeless and doing sex work, he said, which means they’re at risk and have especially high barriers to medical care.
“This is a problem which is affecting the United States as a whole, and in many ways, I think that this is another reverberation of our epidemic of substance abuse and homelessness, which everyone in Seattle is familiar with, at some level,” Golden said.
To counteract the spread of syphilis and other STIs, local public health officials are investing in a strategy you might recognize from the Covid pandemic: contact tracing. It works nearly the same way.
“When we think of a case of chlamydia and a case of Covid, they're actually fairly similar,” said Samantha Matthew, communicable disease supervisor for the Snohomish Health District.
“We're going to gather information about (the patient), where they may have been exposed, and then reach out to those individuals to offer support and provide education,” Matthew said.
Tracing back the infection and testing a patients’ partners is one key part of what can help prevent the spread of syphilis and other STIs.
For STI testing, you can visit your health care provider or one of these providers in King County, Pierce County, and across the state, some of whom will test for free.




